|
|
Video
Transcription By:
Lori A. Eley, RN
Wife of Physician afflicted with RSD / CRPS
Advocate in support of Research and Cure for RSD / CRPS
|
RSD
IN CHILDREN
 |
| Sarah
Young |
Sarah Young:
I want to be a normal teenager.
TV News narrator:
17 year old Sarah Young's battle with RSD, or,
Reflex Sympathetic Dystrophy Syndrome, began
when she was hit with a softball.
 |
| Sarah
Young's Mother |
Sarah's mother:
It took a while to show up, what it was, after
going through multiple doctors who did not...
they were clueless. I had a couple tell me to
cut her leg off, because her leg would be so
blue and ice cold.
UPDATE
September 2007
Nearly three years later, Sarah gave birth to two children
Click HERE
|
TV News narrator:
RSD develops after the body experiences a trauma.
The Sympathetic Nerves, ones that prepare the
body to react to emergencies, misfire and send
constant pain signals to the brain.
Dr. Kirkpatrick:
The mechanism by which an injury triggers RSD
is unclear. The following animation is intended
to give a simplified view of how a relatively
minor injury might lead to RSD. Activation of
the Sympathetic Nervous System following an
injury is part of the fight/flight response
to an emergency situation. This response is
very important for survival.
For example: Firing of the sympathetic nerves
following an injury causes the blood vessels
in the skin to contract, allowing blood to be
shifted to muscle and vital internal organs,
which enables the victim to use his muscle to
get up and escape from danger. Also, decreased
supply of blood to the skin reduces blood loss.
Thus one might expect the skin to turn from
red, due to inflammation, to pale, due to decreased
blood flow following injury. Also, because the
Sympathetic Nervous System causes increased
metabolism and heat production, there is increased
sweat production to cool the body. Ordinarily,
the Sympathetic Nervous System shuts down within
minutes to hours after an injury. The Sympathetic
Nervous System exerts control not only of the
injured part, but of other parts of the body.
Early in the course of RSD, this Regional and
Central control is lost and there is increased
blood flow to the injured area and other parts
of the body. For reasons we do not understand,
individuals who develop RSD the Sympathetic
Nervous System appears to assume an abnormal
function. The sympathetic outflow appears to
cause pain by directly stimulating receptors
on pain fibers. These events are believed to
produce more pain, leading to more stimulation
of the Sympathetic Nervous System, which triggers
another response establishing a vicious cycle
of pain. Thus, we might see changes over time
directly attributable to a abnormal function
of the Sympathetic Nervous System. These changes
include: changes in skin temperature, changes
in the color of the skin, red or bluish discoloration,
changes in sweating, changes in goose flesh
or Piloerection of the skin, and swelling. Most
patients with RSD have more pain expected for
the type of injury they have suffered. They
usually have swelling and discoloration early
in the course of the disease.
Objective Findings
Dr. Kirkpatrick: There
are two important things to remember about the
objective findings sometimes seen with RSD.
First, none of these objective findings for
RSD might be present in a patient with RSD,
especially during the early stages of the disease.
Second, these objective findings tend to be
labile, meaning that they may come and go over
time.
Movement Disorder
These abnormal changes in
the Sympathetic Nervous System seem to be responsible
in some patients for constant pain signals to
the brain. Abnormal function of the Sympathetic
Nervous System leads to Movement Disorder. Pain
is not the only reason why patients have difficulty
moving. Patients state that their muscles feel
stiff and that they have difficulty initiating
movement.
Sometimes blocking the Sympathetic Nervous System
with local anesthetics injected near sympathetic
nerves can lead to a prolonged reversal of this
abnormal sympathetic function, resulting in
improved movement and prolonged relief of pain.
We call this Sympathetically Maintained Pain.
In other cases the pain returns after a series
of sympathetic blocks. In this situation, it
might be possible to obtain a permanent relief
of pain and improve movement by selectively
destroying sympathetic nerves. We call the selective
destruction of sympathetic nerves a Sympathectomy.
In some patients with RSD, blocking the Sympathetic
Nervous System provides little or no relief
of pain. We call this Sympathetically Independent
Pain (SIP). These patients, nonetheless, might
manifest all the findings of abnormal function
of the Sympathetic Nervous System previously
stated.
As RSD progresses over time, especially without
treatment, the disease tends to become more
sympathetically independent and unresponsive
to sympathetic blocks, hence, the importance
of early diagnosis and treatment of RSD. However,
there are some patients who appear to have RSD
that is sympathetically maintained pain (SMP)
for a lifetime, and these patients maintain
a positive response to sympathetic blocks.
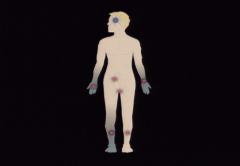 |
| RSD
can spread |
RSD can remain localized
to one region of the body indefinitely. In other
cases, it can spread to other regions of the
body spontaneously or by trauma to other regions
of the body.
For example: In this illustration, RSD has spread
spontaneously to the opposite upper extremity
and to the lower extremity. RSD of the upper
extremity can spread to the face causing problems
with hearing and seeing. Also, RSD of the upper
extremity is sometimes associated with difficulty
in swallowing. RSD of the lower extremities
can be associated with bowel and bladder problems.
Thus the term Total Body RSD has evolved over
the years as we learn more about this disease.
Special Considerations
In Children
Male Narrator:
Pediatric patients present unique challenges.
For example: Children have not had sufficient
time to develop the psychosocial skills necessary
to cope with the pain and suffering due to RSD.
Also, children generally fear needles more than
adults do. Needles are the basic instrument
used to perform sympathetic blocks. This fear
and anxiety in children leads to a lowering
in the children's pain threshold, making nerve
blocks and other medical procedures even more
painful.
Another concern in children relates to cosmetics.
Children might have a greater concern for scar
formation following surgery. These concerns
have led to a great deal of confusion and frustration
among children and their families.
Although there have been no large-scale studies
on the incident of RSD in children, some generalizations
can be made about the children who get this
condition. Published case studies indicate that
the incident of RSD increases dramatically between
9 and 11 years old, and it is found predominantly
in young girls.
During this program we will learn a great deal
about RSD through the voices of children. The
two children in this program are typical for
children who get RSD. Both are female and both
are aged between 10 and 14 years old. These
two children were chosen for another important
reason. These two cases illustrate that not
all RSD is the same. There could be great variability
in the clinical course of the disease as well
as in the response of the condition to treatment.
This variability in RSD has led some to speculate
that there might be different subsets of patients
with this disease.
This videotape has been prepared in consultation
with Dr. Anthony Kirkpatrick and Dr. Dennis
Bandyk. Now please consider this situation:
 |
| Lacey
Booth |
A ten-year-old sprains her
left ankle. Initially, the pain was confined
to the child's left ankle, but over weeks, it
spread to involve the entire left lower extremity.
Associated with the pain the child reported
cold sensation in the leg, whitish to reddish
discoloration of the skin and increased sweating
in the left foot. Also, the patient complained
of increasing sensitivity to light touch causing
pain in the effected region of the leg.
The patient was evaluated by a Pediatrician,
Orthopedist, Rheumatologist and a Neurologist
without arriving at a diagnosis. When examined
at the University of South Florida, lightly
touching or stroking of the skin provoked pain
and she was unable to bear weight with the left
leg.
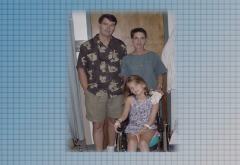 |
| Lacey
was confined to a wheelchair |
The child was confined to
a wheelchair. Using a portable infrared scanner,
the child's left lower extremity was profoundly
colder than the right by 2° degrees centigrade.
Published data and consultant opinions indicated
that a series of one to three sympathetic nerve
blocks may reduce the risk of progression of
RSD. Sympathetic nerve blocks are particularly
urgent when the patient is immobilized with
pain. In this patient's case the child was unable
to bear weight with the left lower extremity
and she was confined to a wheelchair. The child
became progressively worse, despite administration
of pain medications, aggressive Physical Therapy,
and treatment by a Psychologist to help her
better cope with the pain.
The child underwent a series of three lumbar
sympathetic blocks spaced approximately 1 week
apart. The child made only slight improvement
in her condition. At that point a meeting was
held with the family and child to discuss the
child's treatment options. At that meeting an
approach to her treatment was recommended that
ultimately led to a nearly full recovery from
RSD.
Recently, Dr. Kirkpatrick met with the child
and mother for a progress report. This interview
was not recorded in a studio. In fact, Dr. Kirkpatrick
simply placed a camera on the corner of his
desk and began recording. What the interview
might lack in technical quality is more than
made up for in the honest and spontaneous responses
of the child and mother.
(Interview Begins):
Dr. Kirkpatrick:
After we finished doing these blocks on you
we had a meeting, do you remember, in my office?
Lacey:
Yes.
Dr. Kirkpatrick:
Yeah
Lacey:
Mom lost her keys.
Lacey's Mother:
I lost my keys.
Dr. Kirkpatrick:
That's right! That's a good memory, you have
a good memory. You remember. That's right. Now,
see if you can remember that meeting. What do
you think...what was it that I was trying to
emphasize? What do you think I was trying to
communicate at that meeting? Do you remember?
Lacey:
No.
Dr. Kirkpatrick:
You don't remember? Okay. Well, I think one
of the things is that your response to the sympathetic
blocks was nothing to write your mother about.
You seemed like you were doing better, but we
weren't really sure and I said it's better not
to guess about these things...Let's just say
that your response to the blocks was not very
good.
(Lacey nods her head)
Now, you don't remember what I suggested what
we needed to emphasize at that point, do you
remember what I said we need to work on, some
ideas we need to try to develop...do you remember?
 |
| Lacey
and her mother discuss RSD |
Lacey:
You said something about Physical Therapy.
Dr. Kirkpatrick:
Okay.
Lacey:
You said something about needles.
Dr. Kirkpatrick:
Okay. What did I say about Physical Therapy?
Do you remember?
Lacey:
You said I might need to start walking.
Dr. Kirkpatrick:
Yes, and what else did I say?
Lacey:
I don't remember.
Dr. Kirkpatrick:
Okay, alright. I don't know if your mom can
remember. (To Lacey's mom) Do you remember some
of the ideas that we talked about?
Lacey's Mother:
I think we talked about her getting in the pool...um...I'm
not sure I remember...
Dr. Kirkpatrick:
Yes, that was an important meeting to me, and
so it was an important meeting because I wanted
you to get better. And I had a feeling that
I knew what was going to be required to make
you better. And let me tell you what I recall
having said to you and your husband and to Lacey
and that's this: It is understandable why you're
very reluctant to put weight on that foot. It's
very understandable, and your parents needed
to understand, because when you hurt with RSD
it is like no other pain you can imagine, wouldn't
you agree with me?
Lacey:
Uh huh. (Shakes her head yes)
Dr. Kirkpatrick:
And when you complain of pain everyone has to
respect that. I think your mom remembers me
saying that, it ...
Lacey's Mother:
Uh huh.
Dr. Kirkpatrick:
...that it's not that you're not being a big
baby or anything like that, but that it hurts,
and it hurts like no other pain that anybody
can experience, especially a child. And I said
that it's normal not to want to move on it,
it's normal. It's normal not to put weight on
it because, you know, that's how we protect
ourselves when we're hurt, right?
Lacey:
(Nods her head yes)
Dr. Kirkpatrick:
If we kept stepping on glass on the floor, we
would bleed to death, right? So that was very
normal for you to do that. But do you remember
me saying something to the effect that, something
along the lines that...
Lacey:
It wouldn't hurt you.
Dr. Kirkpatrick:
Very good Lacey. You do have a good memory.
You do have a good memory.
Lacey's Mother:
You said, To hurt is not to harm.
Dr. Kirkpatrick:
That's right, we said that. To hurt was not
to harm. But, I also said that you shouldn't
be forced to do that when you're hurting, that
it has to come from you. You have to understand
that, and it isn't easy is it? Be honest?
Lacey:
(Shakes her head no)
Dr. Kirkpatrick:
It's not easy is it?
Lacey:
No.
Dr. Kirkpatrick:
It's not easy because...especially for a child.
I mean, we...as adults...we can put our minds
and say, I believe Dr. Kirkpatrick, and he's
saying it's not going to harm me, it's not going
to break my bones and ruin my tissues and everything.
I could probably talk you mother into that idea,
but try to talk a child into that idea? Wouldn't
you agree with me? It's not as easy to do a
child?
Lacey:
(Nods her head yes and smiles)
Dr. Kirkpatrick:
Because you haven't had a lot of experience
in life. I mean like 10 years. You know what
I mean? Right?
Lacey:
(Nods her head yes and smiles)
Dr. Kirkpatrick:
So, what did you do? I mean, apparently you
did something. How did it happen that you started
moving? Give me an idea, what happened?
Lacey:
Well, umm... mom said we were going to move
from our house if I didn't get out of the wheelchair,
because our house has lots and lots of stairs
and I couldn't do that in a wheelchair. So,
in the pool, I started walking in a pool. And
at first I couldn't do that, and then I could
do that. I started walking up the steps in the
pool with mom holding on to me. Then me and daddy started walking up the steps in the pool.
And then, one day I got out the crutches and
tried to walk, try doing one foot first then
the other. It wasn't really too bad, but it
hurt a lot. So, I went and showed mom. And then
when I was in with mom I did something and it
made it hurt so bad. You remember that, don't
you?
Lacey's Mother:
Uh huh. (Nods her head yes)
Lacey:
She was in the bed. She was watching me going
around the bed, and I was on the corner of the
bed, I'll go, OW! And I guess I hopped a little,
because when I go on crutches I kind of hop.
So, I guess I hopped a little and that really
hurt it, but I just kept doing that, and eventually
I got to where I could walk, slowly.
Dr. Kirkpatrick:
Slowly?
Lacey:
Um, like just little teeny steps. And I got
to where I could walk bigger steps cause I said
to myself, Why walk teeny steps cause it's going
to take you longer to get there, and it's going
to take you longer to get off your feet. So
I started walking big steps, and it wasn't really
bad.
Dr. Kirkpatrick:
Uh huh.
Lacey:
And that's how it happened.
Dr. Kirkpatrick:
How long ago was it roughly? How long ago was
it that you were doing these teeny...because
I didn't see any teeny steps today. I didn't
see any teeny steps. How long ago was it that
you were doing teeny steps, roughly, would you
say?
Lacey:
Um...I don't know.
Lacey's Mother:
It was in July.
Dr. Kirkpatrick:
In July?
Lacey's Mother:
Uh huh. (Nods yes)
Dr. Kirkpatrick:
So, here we are in October...so, we're talking...3
months ago, roughly?
Lacey:
(Nods her head yes)
Dr. Kirkpatrick:
So, you've made some significant improvements
since then. Now, how about this. What about...umm...tell
me about some of the things you're doing nowadays.
I mean, I heard some things about some things
that you've tried that are pretty challenging
physically, right?
Lacey:
(Nods her head yes)
Dr. Kirkpatrick:
Okay.
Lacey:
Um...me and mom have been riding our bikes a
lot.
Dr. Kirkpatrick:
You...you ride a bike a lot?
 |
| Lacey
makes a full recovery |
Lacey:
We have a long dirt road and it's got a big
hill, and I'm the only one that can get up the
hill without stopping now, so... And I do a
lot of running with my friends. And I do Girl
Scouts. And sometimes in Girl Scouts there's
stuff where you run and jump, so that kind of
helps.
Dr. Kirkpatrick:
Uh huh.
Lacey:
And...
Lacey's Mother:
Jump Roping.
Lacey:
I jump rope a lot.
Dr. Kirkpatrick:
Do you? Good for you.
(Interview ends)
Dr. Kirkpatrick:
It is difficult to know exactly how much the
recovery in Lacey's case was due to the series
of sympathetic blocks, and how much was due
to the psychological conditioning that she received.
The adage to hurt is not to harm is an important
principle, however, this principle should be
applied keeping in mind this:
First: The cornerstone in the treatment of RSD
is normal use. The patient needs to mobilize
the effected extremity as much as possible.
Second: Often the Physical Therapist will treat
the patient with RSD with passive manipulation,
causing failure due to extreme pain, even possible
further injury.
Third: learning the non-protective nature of
pain takes time.
Fourth: While encouraging the use of the effected
extremity is critical and may cause increased
pain, it is essential to avoid re-injury.
In contrast to the minimal response to sympathetic
blocks observed in Lacey's case, the next child
illustrates how crucial sympathetic block aid
is to the rehabilitation of a child with Reflex
Sympathetic Dystrophy.
(New case, Amanda)
Imagine that your child is a National Champion
in Gymnastics, even offered a scholarship to
a major University, when, at the age of 10,
all that comes to a crashing end due to a gymnastics
accident. That is the case of Amanda.
Amanda first suffered an injury to her right
wrist; it was a minor sprain of the wrist. The
RSD spread up her arm to include her shoulder.
She required a series of sympathetic blocks.
Unfortunately, the sympathetic blocks did not
provide her with a permanent remission; therefore,
she had to have a Sympathectomy to the right
upper extremity. Subsequently, the patient injured
her left lower extremity, a simple sprain to
the ankle. Again, the symptoms spread up the
leg to include the buttock region as well.
A series of sympathetic blocks were offered.
Again, the patient did not sustain a permanent
remission and had to undergo a sympathectomy
to the left lower extremity as well.
More recently, the patient injured her right
lower extremity and required a series of sympathetic
blocks. Currently, the patient is undergoing
these sympathetic blocks to sustain mobilization
of her right lower extremity.
(Anatomy of nerves demonstration)
Dr. Kirkpatrick:
In order to perform a sympathetic block to the
upper extremity, a needle needs to be inserted
near the neck in order to block the nerve, the
Stellate Ganglia, which sits down, actually,
in the chest. For the lower extremity, the sympathetic
nerves, again, lie along the spine and it is
 necessary to insert a needle into the back,
and come down and block the nerve in this location
here. It is important to recognize that the
sympathetic nerve, indicated here by these little
red dots, are separated from the nerves that
you feel and you move with, your Sensory and
Motor nerves. Therefore, it is possible to block
the sympathetic nerves without blocking the
motor and sensory nerves. Therefore, after a
sympathetic block, the patient should experience
simply a warming of the extremity and not any
change in movement, or in their ability to feel
things. necessary to insert a needle into the back,
and come down and block the nerve in this location
here. It is important to recognize that the
sympathetic nerve, indicated here by these little
red dots, are separated from the nerves that
you feel and you move with, your Sensory and
Motor nerves. Therefore, it is possible to block
the sympathetic nerves without blocking the
motor and sensory nerves. Therefore, after a
sympathetic block, the patient should experience
simply a warming of the extremity and not any
change in movement, or in their ability to feel
things.
(Sympathectomy explained)
Dr. Kirkpatrick:
Sometimes a series of sympathetic blocks is
not sufficient to maintain a permanent improvement
in the patient's condition. Under these circumstances
a permanent block, or sympathectomy, is necessary.
For the upper extremity, one can come in between
the ribs with a scope, find the nerve along
the spinal column, and remove it. For the lower
extremity we have two choices. We can go in
with a needle and dissolve the nerve with a
chemical called Phenol; or surgically, we can
do an excision by going in and actually removing
the nerve from the patient's body.
Another issue of special concern to children
is fear of nerve blocks. In this portion of
the interview, Amanda discusses her experience
with Intravenous Sedation and nerve blocks.
In children, sedation is usually provided during
sympathetic blocks. Combinations of Midazolam
and Propofol have successfully been employed
to relieve anxiety. Unfortunately, larger doses
of these agents are required to prevent movement
during the procedure. This can leave the child
with an unpleasant feeling of a Hang-Over. We
have successfully added small doses of Ketamine,
which intensifies the sedation, decreases the
amount of Midazolam and Propofol required, and
thus prevents the feeling of hang-over. In addition,
recent studies showed that small doses of Ketamine
actually increased breathing, thus increasing
the safety margin for deep sedation.
Let's hear from Amanda about her experience
with deep sedation and nerve blocks.
(Interview with Amanda about sedation and blocks
begins)
Dr. Kirkpatrick:
Now, one of the things that you know, again
we're dealing with children, is the fear, the
fear of having treatments and you've been through
a lot, a lot of nerve blocks. I mean, you added
them up young lady, we're talking big time.
I mean, if you said, I had 50 or 60, I mean,
I didn't do all those, but you know, you add
them up. There's been a lot of nerve blocks,
sympathectomies, upper and lower.
Amanda:
Yeah.
 |
| Amanda
Alberigi and mother discuss RSD |
Amanda's Mother:
Yes, Right.
Dr. Kirkpatrick:
I mean, there's been a lot going on here. I'm
just wondering do the nerve blocks scare you?
Amanda:
No. The first time maybe, yeah, but...
Dr. Kirkpatrick:
After a while...
Amanda:
I trust you.
Dr. Kirkpatrick:
Tell us, not about the trust; tell us about
the block. You know, when we treat you we use
a medication. We don't use it alone; we use
it with a sedative, okay?
Amanda:
Uh huh.
Dr. Kirkpatrick:
Versed, Midazolam...
Amanda's Mother:
Versed.
Dr. Kirkpatrick:
And we use Ketamine. And the reason we use Ketamine
is because it helps keep you breathing. And
one thing we know about children, young people,
they need a lot of oxygen. And I mean they burn
oxygen like crazy and if they don't get oxygen,
they go blue real fast, you know? So, Ketamine
is the drug we use. Now, when we give you Ketamine
is there anything about it that you, uh...for
example: some people dream, some people don't.
Do you ever dream with it?
Amanda:
No.
Dr. Kirkpatrick:
Do you ever have any...do you recall any...uh...well...not
dreams, but just the funny feelings like colors
or anything like that? No?
Amanda:
No.
Dr. Kirkpatrick:
No? You're just out?
Amanda:
Out for the count.
Dr. Kirkpatrick:
You're out for the count.
(Interview discussion about sedation and blocks
ends)
Dr. Kirkpatrick:
It is worth emphasizing that Ketamine should
never be used alone. It should be used with
other sedatives; otherwise the child may awaken
in an uncomfortable state. The IV should be
inserted in an area other than the procedure
room. The procedure room can be a very threatening
environment. In addition, parents may unintentionally
generate fear in the child if they fear needles
themselves. Therefore, it might be best not
to have the parent present during the insertion
of an IV.
Cosmetics, or scar formation after surgery,
is another concern to children. Amanda addresses
some of these concerns during the interview.
(Interview with Amanda about cosmetics/scar
formation begins)
Dr. Kirkpatrick:
Lets talk about another thing that you, only
you can...probably more than anybody else I've
ever seen...perhaps help understand a concern
that children have. And that is, you eventually...after
the Phenol didn't take long enough...you ended
up getting a surgical, a surgical sympathectomy
done. And of course, young people, appropriately
fear a scar. I mean, you know, bikini's are
sort of like in and that sort of thing.
Amanda:
(Nods her head yes)
Dr. Kirkpatrick:
So Amanda, tell me about that.
Amanda:
My, uh...the scars don't bother me really. I
don't even realize they're there sometimes.
I mean, the ones that I have under my arm, they're
healed pretty well, except the chest tube one.
It's still there, but...
Dr. Kirkpatrick:
It's still there?
Amanda:
...and they don't bother me.
Dr. Kirkpatrick:
Now suppose you want to make an appearance.
I'm sure if it was you or some other child,
that there's a way you can cosmetically conceal
it a little bit. Uh...I've been told, of course
I'm no expert at this, but I've been told...
like... for example when women have breast implants,
that they can put this little tape and stuff
on it.
Amanda:
Uh... that's the most painful thing I've ever
had to go through in my life.
Amanda's Mother:
We've tried it.
Dr. Kirkpatrick:
Oh, you've tried it. Okay.
Amanda:
We're not doing that.
Dr. Kirkpatrick:
Well tell us. What happened?
Amanda:
I did it with my chest tube one and it hurt.
Dr. Kirkpatrick:
Oh, it's painful? Really?
Amanda:
When you have to rip it off it hurts. Yeah,
it hurts!
Dr. Kirkpatrick:
Oh, in other words you put it on temporarily
for whatever the...
Amanda:
Right. 24 hours.
Amanda's Mother:
Right. It's a patch and you wear it for 24 hours
and you have to take it off. It did reduce the
swelling and the color, because it was a raised
scar... and it healed from the inside out...so
it was raised. To where the one on her stomach,
which is still very sensitive, we haven't even
attempted that. But she kept Vitamin E as well
as 50 sun protector, being out in the sun during
the summer...
Amanda:
I show my scars.
Amanda's Mother:
...and she doesn't hide them. She doesn't let
them bother her.
Dr. Kirkpatrick:
Yeah, yeah...well let me ask you this now, if
I understand, because I've never seen this technique.
Amanda:
It's called a silicone patch.
Dr. Kirkpatrick:
That's what it's called, a silicone patch?
Amanda:
Uh huh.
Dr. Kirkpatrick:
Now, does it leave like...you put it on ...it
has to be on for 24 hours and you take it off?
Does it leave something there on your skin?
Is that what it's supposed to do?
Amanda's Mother:
I don't know.
Amanda:
You have to replace them every 24 hours.
Dr. Kirkpatrick:
Every 24 hours?
Amanda and her Mother together:
Yes, yes. Replace them for 30 days.
Dr. Kirkpatrick:
So, it's not a patch you put on and leave on
to cover it up, but when you take it off, that's
the final product?
Amanda:
It reduces the scar more and more.
Amanda's Mother:
It shrinks it.
Dr. Kirkpatrick:
Oh. It shrinks the scar. Oh, I see. But what
you're saying when you gave it a try just for
fun, whatever, it was painful taking it off.
Amanda:
Yeah. It feels like ripping a band-aid off,
just ten times bigger.
Dr. Kirkpatrick:
Right, right...
Amanda's Mother:
Because the patch is about that square, 5 by
3 square.
Dr. Kirkpatrick:
I see. So the Sympathectomy to the left lower
extremity was done about 14 months ago...
Amanda:
No.
Amanda's Mother:
No, no, April 2nd.
Dr. Kirkpatrick:
April 2nd...
Amanda's Mother:
April 2nd, 2001. Seven months ago.
Dr. Kirkpatrick:
7 months ago. Now, can you show your scar here
so we can see it?
Amanda:
Yes.
Amanda's Mother:
Don't show the belly button ring.
Dr. Kirkpatrick:
Oh yeah. Let me see if we can get a little close-up
of that. There we go. Alright. So, that's the
scar and you did say that you tried to apply
that...
Amanda:
Not to this one.
Amanda's Mother:
Just Vitamin E and sunscreen.
Dr. Kirkpatrick:
Yeah. Without getting too private, is there
a...can you show the other one?
Amanda:
Here's one.
Dr. Kirkpatrick:
Yeah, let's see. That's only one, there should
be three.
Amanda:
There's one under my breast.
Amanda's Mother:
But you can't hardly see it.
Dr. Kirkpatrick:
You don't have to show us the one under ...
Amanda's Mother:
You can't hardly see them.
Dr. Kirkpatrick:
You don't even see them. Put your finger on
the one there. There's one there. Let me see
if I can zoom in on that. Let me go up there.
Let me see. There's one up there; that little
guy.
Amanda's Mother:
That's where the chest tube was.
Dr. Kirkpatrick:
That's where the chest tube was...
Amanda:
...and then there's...you can't see the other
ones...
Amanda's Mother:
No it's...
Amanda:
You can't even see it.
Amanda Mother:
No, it's...you can't even see it.
Dr. Kirkpatrick:
So she's only left with 2 scars. Well, that's
interesting. So, the one that leaves most of
the scar appearance is really the one that is...
Amanda:
On my stomach...
Dr. Kirkpatrick:
On your stomach, yeah. So that's important you
know. I mean, that scar appearance is really
the one that is...
Amanda:
On my stomach.
Dr. Kirkpatrick:
On your stomach, yeah. So, that's important
you know. I mean that we recognize and be able
to tell young people, Hey, if you're going to
have a surgical sympathectomy, you're going
to get into something a little more substantial.
Amanda:
Uh huh.
Dr. Kirkpatrick:
Now tell us this, you know you've had both.
When you look back at your recovery from the
two, which one was the more difficult one after
surgery to deal with, would you say?
Amanda:
The one in the upper area.
Dr. Kirkpatrick:
It was? Why is that?
Amanda:
Because I was in ICU for 24 hours with a chest
tube.
Dr. Kirkpatrick:
With a chest tube?
Amanda:
And that was rough.
Dr. Kirkpatrick:
That was rough?
Amanda:
That was very rough.
Dr. Kirkpatrick:
And they gave you pain medicine for that?
Amanda:
They gave me Morphine, but I didn't want it
anymore. So, I was just taking Tylenol.
Dr. Kirkpatrick:
Yeah, because it makes you kind of dopey? Is
that the reason?
Amanda:
No. It made me sick.
Dr. Kirkpatrick:
It made you sick, like nauseated?
Amanda:
Oh yeah.
Dr. Kirkpatrick:
Yeah, um...but... well of course, we all know
that for the lower one...for the lower one...on
the lower part...that one, you were out the
next day I believe, out the door.
Amanda:
Uh huh.
Dr. Kirkpatrick:
You know, this is kind of interesting, because
you know what? In adults, it's the other way
around.
Amanda's Mother:
That's what Dr. Bandyk told us. He said, My
patients don't usually go home for 4 days.
Dr. Kirkpatrick:
Yeah. They're out of the hospital faster for
the upper extremity sympathectomy than for the
lower one. And that's a difference, and that's
a difference that's very important.
Amanda's Mother:
We were in the hospital for 5 days for the upper
and less than 24 hours for the lower. And she
was up walking around the same night that she
had the lower one.
Dr. Kirkpatrick:
Yeah. What I'm planning to do here is, you know,
I have the video of that little worm they took
out of you.
Amanda's Mother:
Yes.
Dr. Kirkpatrick:
Did I send you that video?
Amanda's Mother:
Yes you have.
Amanda:
Yes.
 |
Laughter
occurs when the family learns that
Amanda's surgery will be part of the video
program |
Dr. Kirkpatrick:
I'm going to try to get that inserted in here
so that we can look at it. Now, is there anything
else that we could... have we missed anything
from the mother's point of view? What do you
think? Is there anything else that's important
having gone through all of this?
Amanda's Mother:
Think positive and be strong. Trust your doctor.
I mean, they're the only ones that know what's
really right. I mean, and if she wasn't comfortable
in any of the decisions...I always let her be
involved in the decisions, because that's...it
was her body, it's her that it's happening to,
not me. So, I can't be the one to say, well
this is going to fix it, let's do it , and I
let it be her decision. So I think it's important
she, you know, each child needs to. But they
need to know the repercussions of, you said,
the scars, you know? Are they so vain they don't
want the scars, and do they want to just have
the pain? Do they just want to deal with it
or do they want to get better.
Dr. Kirkpatrick:
Yeah.
Amanda's Mother:
And knowing that this was the best way to get
better, we made the decision, and we made a
very reasonable decision to have it done.
Dr. Kirkpatrick:
So Amanda, what's your take on it? Do you agree
with that?
 |
Amanda
is cured of RSD in her right upper
extremity by sympathectomy |
Amanda:
I do. You've got to be positive, you can't think
negatively.
Dr. Kirkpatrick:
Yeah.
Amanda:
You can't think negatively.... (Inaudible)
Dr. Kirkpatrick:
Right.
(Interview with Amanda ends)
(Dr. Bandyk discusses sympathectomy)
 |
Dr.
Dennis Bandyk explains the risks,
limitations and potential benefits |
Dr. Bandyk:
It must be emphasized when undertaking more
invasive approaches to pain management such
as sympathectomy, that the benefits must be
carefully weighed against the risks. Recently,
we reported on a large series of patients with
RSD at the University of South Florida that
had undergone sympathectomy. Over 3/4 of the
patients had long-term benefits from the procedure.
However, other patients did not obtain significant
long-term benefits despite very careful selection
for sympathectomy.
Furthermore, it should be emphasized that there
is little published data on sympathectomy in
children. Therefore, extra caution is prudent
when considering sympathectomy in children until
more data becomes available.
The selective use of these invasive treatments
must be by a very experienced physician. Before
considering a sympathectomy, a child should
be offered a series of pure sympathetic blocks
to help facilitate an informed consent about
what to expect from a sympathectomy. An epidural
block is not a pure sympathectic block.
Before considering an invasive procedure the
family should be encouraged to obtain a second
opinion to ensure that all lesser invasive therapies
have been tried. In Amanda's case, her multiple
extremity RSD consistently forced her to be
absent from school within one week after each
sympathetic block. Pain medications, aggressive
physical therapy and extensive psychological
counseling all failed to control her RSD symptoms.
Now it appears that she has been cured of RSD
in both her right upper and left lower extremities
following sympathectomy to those regions of
her body.
Children will fall into several groups. First
are those who are permanently cured by treatment.
The second is a group of children whose conditions
are improved, but then show a high recurrence
of RSD. Fortunately each subsequence occurrence
of RSD seems less severe. A third and relatively
small group of children with RSD get progressively
worse despite treatment and require aggressive
intervention, even sympathectomy. In this last
group of children with the most severe form
of RSD, physicians may procrastinate and wait
until the skin of the extremity turns from blue
to black, indicating irreversible tissue loss,
before considering a sympathectomy.
Once a disease is allowed to progress to this
advanced stage, it may be too late for a sympathectomy
to provide any improvement in tissue perfusion,
or prevent the need for an amputation.
A sympathectomy should be considered before
such severe dystrophic changes occur in the
tissues of a child with RSD. It is often difficult
to know in advance if a child falls into this
more severe form of RSD, therefore, vigilance
is required in following the clinical course
of RSD in children, in order to achieve the
best outcome.
Recently, the surgical technique for sympathectomy
has been modified to minimize scar formation.
For example, the need for insertion of a post-operative
chest tube is being eliminated in some patients.
And the laparoscope is now being used to perform
Lumbar sympathectomy of the lower extremity
as well.
(Dr. Bandyk's discussion ends)
(Dr. Kirkpatrick's discussion begins)
Dr. Kirkpatrick:
Some children with RSD improve with conservative
treatment. Indeed, the available pediatric literature
supports the notion that a high percentage of
children will improve with active mobilization
of the affected extremity and psychosocial conditioning
alone. There is a definite art to guiding a
child through a step-wise return to weight bearing
and mobilization of the effected extremities,
and for helping them to understand the difference
between protective and non-protective pain.
As shown in this video program some children
benefit significantly from pool exercises.
According to a recent study at Harvard Medical
School, one needs to remain vigilant for a recurrence
when a child goes into remission following a
bout with RSD. In that study, recurrent episodes
of RSD in children occurred in up to 40% of
patients, however, most of these recurrent episodes
were milder than the initial episode.
A variety of medications are helpful for individual
children, but there is no perspective pediatric
literature on specific effectiveness of most
of these agents for this type of pain found
with RSD. Trials of anti-depressants such as
Nortriptyline might be useful as adjuncts for
sleep in many patients. Anticonvulsants such
as Gabapentin are sometimes helpful. Several
patients have had good responses to a short
course of Prednisone early in a flare-up; others
have not. Clearly, further research is needed
to determine what is the most effective treatment
options for children.
Another important point, in several case series,
a high percentage of children with RSD have
been very involved in sports, dance and gymnastics.
Indeed, the thought of gymnastics competition
often conjure images of major trauma as shown
in these short video clips. It must be emphasized,
however, that most children that engage in gymnastics
or similar sports do not get RSD. The fact is,
RSD can be triggered by a relatively minor injury.
We would like to give special thanks to Lacey
and Amanda for the significant contribution
they've made to educating us about RSD.
Male Narrator:
Some key points made in this video are worth
emphasizing:
The pathophysiology of RSD is uncertain. The
animation presented during the early part of
the video program is at best an over simplification
of how RSD develops following injury. In fact,
some refer to RSD as a Complex Regional Pain
Syndrome to avoid the implication that the disease
has to involve a reflex of the Sympathetic Nervous
System. These two pediatric cases illustrate
that there is great variability in the clinical
course of the disease as well as variability
in the response to treatment. The importance
of time in treating RSD needs to be stressed.
Do not expect change overnight. Active participation
of the child is crucial.
It needs to be emphasized that this video is
a case-report about two children who have had
to struggle with RSD. The video program is not
intended to be a comprehensive review of the
treatment options available for children with
this disease.
The video glossed over fairly quickly medication
trials, cognitive and behavioral approaches
to pain, which are the meat that help the majority
of children with RSD.
As with sympathectomy, there are other invasive
treatments such as Spinal Cord stimulation that
might be applicable to only a small minority
of children with RSD. Because everyone is different,
the information expressed in this video program
cannot and should not be used to diagnose or
treat individual health problems in patients
with RSD. The treatment must be individualized
by a health professional.
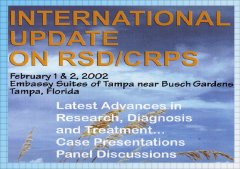 |
This
video program underwent extensive
peer review at the international symposium
held at the University of South Florida |
A 30-minute version of this
video was presented and peer-reviewed by an
international panel of experts on RSD, at the
International Update on RSD / CRPS, held at the
University of South Florida. As a result of
the comments received by this panel, the video
was expanded to 40 minutes in order to cover
a broader range of issues in the diagnosis and
treatment of RSD.
For complete guidelines for the Diagnosis and
Management of RSD, please refer to the Clinical
Practice Guidelines available on the Internet
in English, Spanish and French published by
the Reflex Sympathetic Dystrophy Syndrome Association
of America and by the International Research
Foundation for RSD / CRPS. The Scientific Advisory
Committee on RSD wrote these guidelines.
We hope you found this overview of RSD in children
helpful. |
|
|
HOME | MENU | CONTACT
US
The International Research Foundation
for RSD / CRPS is a
501(c)(3) (not-for-profit) organization in the United States of America.
Copyright © 2003 International
Research Foundation for RSD / CRPS.
All rights reserved.
For permission to reprint any information on the website, please contact
the Foundation.
|

